Introduction
Accurate coding represents the foundation of successful medical practice management. When providers submit claims for services like injections administered during office visits, specific rules apply to maintain billing integrity. The M14 code works as an important guideline in these situations, helping healthcare practices avoid denials in payment and compliance issues.
This article tells in brief about the M14 code’s purpose, application, and its impact on medical billing processes. Understanding M14 helps medical professionals maximize appropriate reimbursement while adhering to payer requirements for injection services provided during office encounters.
What is M14?
M14 is a Medicare Remittance Advice Remark Code (RARC) that states: “No separate payment for an injection administered during an office visit, and no payment for a full office visit if the patient only received an injection.”
This code enforces a fundamental reimbursement principle: preventing duplicate payments when a service is already included within another billable procedure. M14 specifically addresses the relationship between:
- Office visits (Evaluation and Management services)
- Administration of injections
- The injectable medications themselves
The Bundling Concept
M14 functions on the concept of “bundled services” – related procedures that payers view as components of a single reimbursable service. When a patient receives an injection during an office visit, Medicare and many private insurers apply specific rules to determine whether separate payment for both services is appropriate.
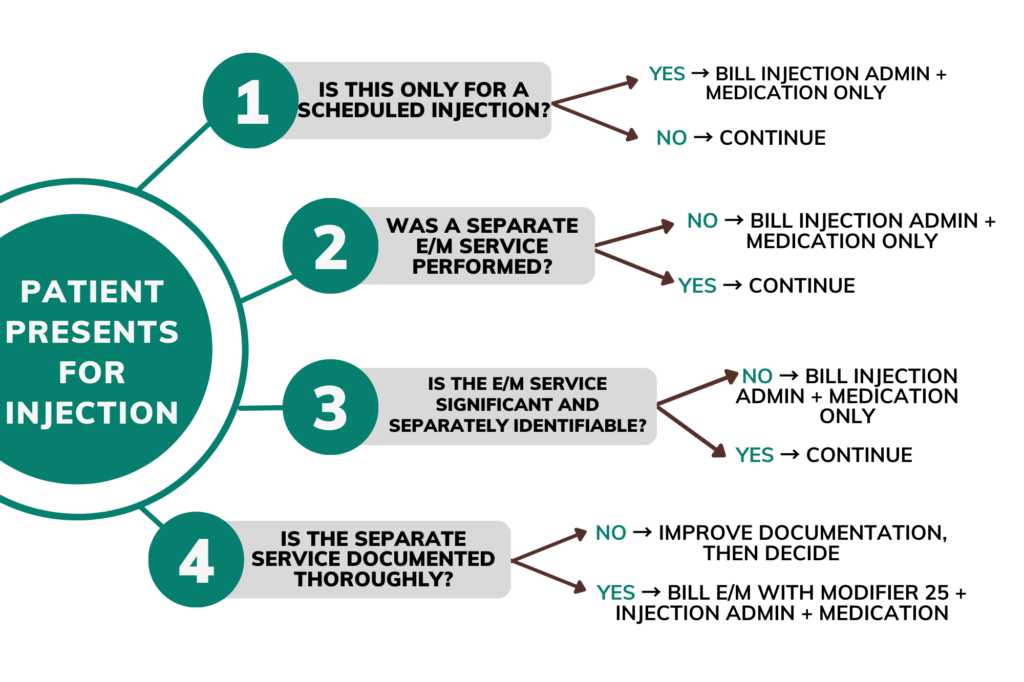
The basic principle behind M14 states:
- If a patient visits solely for an injection, only the injection administration and medication should be billed
- If the office visit includes additional, significant services beyond the injection, both may be billable with proper documentation and modifier use
Bundled Services Concept
| Standard Office Visit Components | Injection Administration Components |
| Patient assessment | Preparation of injection |
| Medical history review | Administration technique |
| Physical examination | Post-injection monitoring |
| Medical decision-making | Disposal of materials |
| Documentation | Documentation of administration |
When services overlap, M14 prevents duplicate payment for the same clinical work
M14 in Practice: Common Billing Scenarios
When a patient arrives exclusively for a scheduled injection (such as B12, allergy shots, or regular medications):
| Service | Correct Billing Approach |
| Office Visit (E/M service) | Do not bill |
| Injection Administration | Bill appropriate CPT code (e.g., 96372) |
| Injectable Medication | Bill appropriate J-code or drug code |
Example: A patient with pernicious anemia receives monthly B12 injections. For this routine visit, bill only the injection administration (96372) and the medication (J3420). No E/M service should be reported.
Scenario 2: Significant, Separate Service with Injection
When a patient receives an evaluation that goes beyond the injection itself:
| Service | Correct Billing Approach |
| Office Visit (E/M service) | Bill with modifier 25 |
| Injection Administration | Bill appropriate CPT code (e.g., 96372) |
| Injectable Medication | Bill appropriate J-code or drug code |
Example: A patient arrives for a scheduled testosterone injection but also reports new fatigue symptoms. The physician performs a detailed evaluation of these symptoms, orders blood work, and adjusts the patient’s treatment plan. This visit involves:
- 99213-25 (Office visit, established patient)
- 96372 (Injection administration)
- J1071 (Testosterone cypionate)
Common M14-Related Billing Challenges
Healthcare providers frequently encounter several issues related to M14 denials:
1. Documentation Shortfalls
Medical practices often overlook the need to clearly document how the evaluation and management (E/M) service is separate from the injection procedure during the same visit. Medical records must clearly show:
- The separate nature of the evaluation
- Medical necessity for services beyond the injection
- The provider’s thought process and decision-making
2. Modifier 25 Misapplication
The modifier 25 (significant, separately identifiable E/M service) frequently causes confusion. This modifier should be used only when:
- The E/M service exceeds the basic pre/post-service work in relation with the injection
- The patient’s condition requires evaluation beyond what’s needed for the injection
- The documentation supports the additional work performed
3. Routine Injection Visit Upcoding
Some practices incorrectly bill E/M services for every injection visit, regardless of complexity. This pattern may trigger:
- Claim denials
- Payer audits
- Compliance issues
- Financial penalties
Best Practices for M14 Compliance
Documentation Excellence
Strong documentation forms the backbone of appropriate coding. For injection visits, records should clearly specify:
- The reason for the visit and chief complaint
- Any separate medical concerns addressed
- Assessments performed beyond what’s needed for the injection
- Medical decision-making processes
- Treatment plans and follow-up instructions
Staff Education
Front-line staff and billing teams need ongoing training about:
- The difference between injection-only visits and medically necessary evaluations
- Proper use of the modifier 25
- Documentation requirements for separate services
- Common payer guidelines regarding injections
Coding Verification Process
Implement a verification system to catch potential M14 issues before submission:
- Review encounters where both injections and E/M services were billed
- Verify supporting documentation for separate services
- Check for appropriate modifier use
- Confirm medical necessity for all billed services
Scenario: M14 in Action
Case 1: The Routine Allergy Shot
Scenario: A patient visits for a weekly allergy immunotherapy injection.
Initial Billing Error: The practice billed both the injection administration (95115) and a level 2 office visit (99212).
Result: Claim denied with M14 remark code.
Correction: Removed the E/M code and resubmitted with only the injection administration code. The claim was then processed for payment.
Lesson: Scheduled, routine injections without additional medical concerns should not include E/M services.
Case 2: The Complex Injection Visit
Scenario: A patient arrives for a scheduled Depo-Provera injection but reports experiencing unusual side effects since the last injection.
Billing Approach: The provider conducted an expanded problem-focused history and examination addressing the patient’s side effects, and documented the decision-making process related to continuing the current medication plan.
Correct Coding:
- 99213-25 (Office visit, established patient)
- 96372 (Injection administration)
- J1050 (Depo-Provera)
Result: Clean claim payment due to appropriate documentation and modifier use.
Lesson: When a separate, significant service occurs during an injection visit, both services may be billable with proper documentation and modifier application.
Practical Application: M14 Billing Decision Tree
Use this decision tree to determine the appropriate billing approach for injection visits:
Financial Impact of M14 Compliance
Proper management of injection billing affects practice revenue in several ways:
Revenue Protection
Accurate coding prevents:
- Claim denials requiring staff time to resolve
- Payment delays affecting cash flow
- Recovery audits and potential repayment obligations
Appropriate Reimbursement
Understanding M14 helps practices:
- Receive payment for legitimately separate services
- Apply modifiers correctly to support medical necessity
- Document effectively to support billing decisions
Audit Readiness
Practices with strong M14 compliance:
- Maintain consistent documentation patterns
- Show appropriate use of modifiers
- Demonstrate clear distinction between bundled and separate services
Conclusion
The M14 code plays an important role in medical billing integrity by preventing duplicate payments for injection services during office visits. Healthcare providers who understand this code’s application can:
- Submit accurate claims aligned with payer requirements
- Document appropriately to support billing decisions
- Avoid unnecessary denials and payment delays
- Maintain compliance with billing regulations
Medical practices benefit from regular education on injection billing rules, thorough documentation practices, and internal auditing processes to verify M14 compliance. By following these guidelines, providers can optimize reimbursement while adhering to proper billing standards.